(1) Pardon my French, but this is a big [bleep]ing deal. Via Matt Margolis, here are revised CDC best estimates for COVID-19 epidemiological parameters (Table 1, “Scenario 5”). Parameter values are based on data received by CDC prior to 4/29/2020
Their R0=2.5 (remember, R-naught is the reproductive number absent any intervention). Percent asymptotic infections is 35%.
Age cohort Fatality Hospit. of which ICU
Under 50 0.05% 1.7% 21.9%
50-64 0.2% 4.5% 29.2%
Over 65 1.3% 7.4% 26.8%
Overall 0.4% 3.4% N/A
Also according to the report, about three-quarter of patients in the ICU need mechanical ventilation of some sort, regardless of age group.
Now wait a second, you say. According to worldometers, the cumulative documented infections on April 29 were 1,064,194, with 61,655 deaths. That’s an overt case fatality rate (CFR) of 5.79% — while now CDC is talking a CFR of 0.4% CFR, and an infection fatality rate of 0.26% [that is, 0.4%*(100%-35%)]. How come?
Well, “overt” or “documented” is the operative word here. These number imply a Dunkelziffer/undocumented infection rate of about 22 times the known infection rate. (This ratio is actually within the uncertainty band of the revised Santa Clara County community sampling study. (Bendavid, Ioannides et al. from Stanford).
As I reported here on May 5, German virologist Hendrik Streeck, from his whole-community testing of the hard-hit German town of Gangelt, inferred an IFR of “0.36%, but possibly as low as 0.24%”. He at the time suggested the ratio between the overt CFR and 0.36% as a guesstimate for the Dunkelziffer. It increasingly looks like Streeck, Ioannides, and the CDC are all on the same page to within overlapping uncertainties.
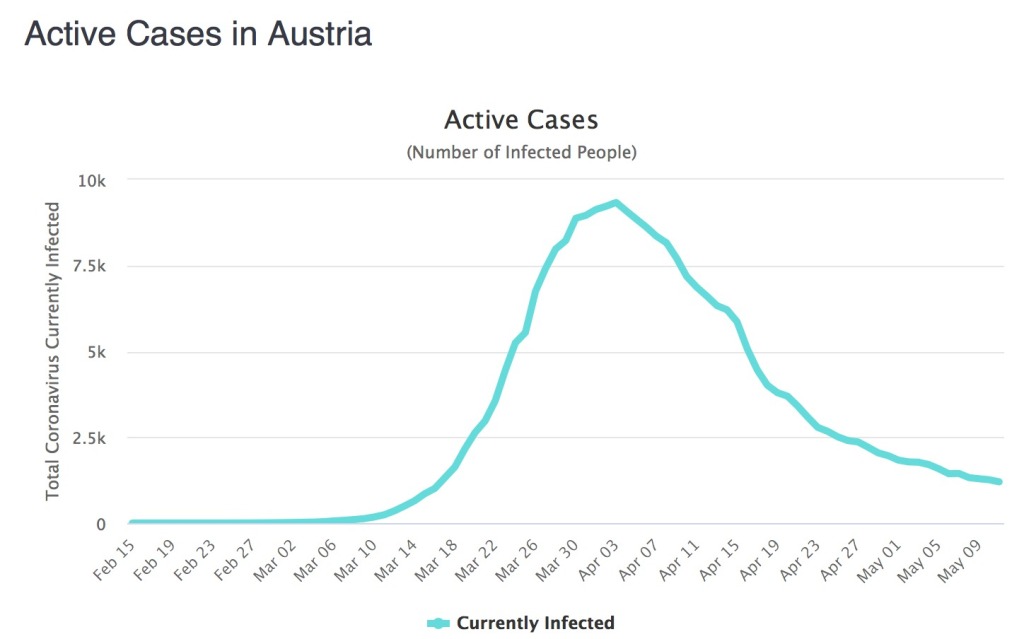
Back in March, the single biggest “known unknown” the decision makers had was precisely the Dunkelziffer. Would they have decided on hard lockdowns based on a 0.26% IFR? Chances are, many countries would have hewn a course closer to Sweden’s. But decisions made “in the fog of war”, as a member of our local ad hoc planning commission described it, are easy to second-guess with 20:20 hindsight. Back then, our own commission applied case fatality rates by age cohort reported from China to our much “younger” population pyramid, and arrived at an “if we do nothing” back-of-envelope upper limit 20,000 dead before herd immunity would be reached. Based on what we know with benefit of hindsight, it would probably have been more in the 3,000-8,000 range. As of today, after a strict but comparatively brief lockdown and a phased reopening, we have fewer than 300 dead out of a population of 9.15 million. So it is possible that the lockdown saved thousands of lives here — but it could be that our thankfully small mortality is thanks as much to our sunny climate and comparatively outdoors lifestyle as to any human intervention.
What we can tell now, however, is that extended lockdowns have long outlived any epidemiological purpose they ever might have had. At this point, their collateral mortality will well exceed any residual epidemiological benefit they might still have. Besides, in the states and countries that have reopened, the sky isn’t falling.
(2) This new paper in the top-tier journal CELL https://doi.org/10.1016/j.cell.2020.05.015 (h/t: LittleOldLady) and this press release about it, in layperson-friendly languagee (h/t: Jeff Duntemann) have some very hopeful news about COVID19 and immunity. But the big shocker to me was buried further down:
The teams also looked at the T cell response in blood samples that had been collected between 2015 and 2018, before SARS-CoV-2 started circulating. Many of these individuals had significant T cell reactivity against SARS-CoV-2, although they had never been exposed to SARS-CoV-2. But everybody has almost certainly seen at least three of the four common cold coronaviruses, which could explain the observed crossreactivity.
It is still unclear, though, whether the observed crossreactivity provides at least some level of preexisting immunity to SARS-CoV-2 and therefore could explain why some people or geographical locations are hit harder by COVID-19.
“Given the severity of the ongoing COVID-19 pandemic, any degree of cross-reactive coronavirus immunity could have a very substantial impact on the overall course of the pandemic and is a key detail to consider for epidemiologists as they try to scope out how severely COVID-19 will affect communities in the coming months,” says Crotty.
Most common colds are caused by rhinoviruses, but actual coronaviruses account for a minority of them. “Cross-reactivity” is immunology-speak for where exposure to one antigen results in at least a partial immune response to related antigens. What Edward Jenner achieved — inoculating people with the relatively innocuous cow pox and thus giving them immunity to the far more dangerous smallpox — is an example of strong cross-reactivity. [*] Hmm, could be be seeing inoculation with common-cold coronaviruses?
Staying on the immunity topic, reader Cathe Smith drew my attention to this recent paper in NATURE Communications: https://doi.org/10.1038/s41467-020-16505-0 Let me just give a teaser:
To address the urgent need for a medical countermeasure to prevent the further dissemination of SARS-CoV-2 we have employed a synthetic DNA-based vaccine approach. Synthetic DNA vaccines are amenable to accelerated developmental timelines due to the ability to quickly design multiple candidates for preclinical testing, scalable manufacturing of large quantities of the drug product, and the possibility to leverage established regulatory pathways to the clinic. Synthetic DNA is temperature-stable and cold-chain free, important features for delivery to resource-limited settings7. Specifically for the development of a COVID-19 vaccine candidate, we leveraged prior experiences in developing vaccine approaches to SARS-CoV8, and our own experience in developing a MERS-CoV vaccine (INO-4700)9,10, as well as taking advantage of our vaccine design and manufacturing pathway previously utilized for the Zika vaccine candidate, GLS-570011, which was advanced to the clinic in under 7 months. INO-4700 and GLS-5700 vaccines are currently in clinical testing.
[*] Cross-reactivity is not limited to pathogens. People who have an allergic reaction to a given antibiotic (e.g. a penicillin), and who are switched to a different antibiotic (e.g., a cephalosporin) may sometimes develop a cross-reaction to the latter (which is from a different “branch” of the same chemical family, beta-lactams).
ADDENDUM: New CDC report on transmission: easily from person to person, less easily via fomites (intermediate objects), unlikely via pets. John Campbell clarifies.
And via Dr. Seheult, an analysis piece in THE LANCET Diabetes and Endocrinology about vitamin D and COVID19.
https://doi.org/10.1016/S2213-8587(20)30183-2
Moneygrafs:
A growing body of circumstantial evidence now also specifically links outcomes of COVID-19 and vitamin D status. SARS-CoV-2, the virus responsible for COVID-19, emerged and started its spread in the Northern hemisphere at the end of 2019 (winter), when levels of 25-hydroxyvitamin D are at their nadir. Also, nations in the northern hemisphere have borne much of the burden of cases and mortality. In a cross-sectional analysis across Europe, COVID-19 mortality was significantly associated with vitamin D status in different populations. The low mortality rates in Nordic countries are exceptions to the trend towards poorer outcomes in more northerly latitudes, but populations in these countries are relatively vitamin D sufficient owing to widespread fortification of foods. Italy and Spain are also exceptions, but prevalence of vitamin D deficiency in these populations is surprisingly common. Additionally, black and minority ethnic people—who are more likely to have vitamin D deficiency because they have darker skin—seem to be worse affected than white people by COVID-19. For example, data from the UK Office for National Statistics shows that black people in England and Wales are more than four times more likely to die from COVID-19 than are white people.
[…]
Rose Anne Kenny (Trinity College Dublin, University of Dublin, Ireland) led the cross-sectional study into mortality and vitamin D status and is the lead investigator of the Irish Longitudinal Study on Ageing (TILDA). She is adamant that the recommendations from all public health bodies should be for the population to take vitamin D supplements during this pandemic. “The circumstantial evidence is very strong”, she proclaims regarding the potential effect on COVID-19 outcomes. Adding, “we don’t have randomised controlled trial evidence, but how long do you want to wait in the context of such a crisis? We know vitamin D is important for musculoskeletal function, so people should be taking it anyway”. Kenny recommends that, at the very least, vitamin D supplements are given to care home residents unless there is an extremely good reason not to do so.
Adrian Martineau (Institute of Population Health Sciences, Barts and The London, Queen Mary University of London, UK), lead author of the 2017 meta-analysis has joined with colleagues from universities around the UK to launch COVIDENCE UK, a study to investigate how diet and lifestyle factors might influence transmission of SARS-CoV-2, severity of COVID-19 symptoms, speed of recovery, and any long-term effects. They aim to recruit at least 12 000 people and to obtain interim results by the summer. Despite his enthusiasm for the study, Martineau is pragmatic: “At best vitamin D deficiency will only be one of many factors involved in determining outcome of COVID-19, but it’s a problem that could be corrected safely and cheaply; there is no downside to speak of, and good reason to think there might be a benefit”.
And now Dr. Anthony Fauci has warned that staying closed for too long could cause irreparable damage.